This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 75 year old male came to casualty with chief complaints
Fever since 2 days , ALTERED SENSORIUM SINCE today
History of SHORTNESS OF BREATH SINCE 2 DAYS.
HISTORY OF DRY COUGH on and off SINCE 8 months
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1 year back and then started refusing to sleep in his room after the demise of his wife patient had c/o decreased hearing on his left ear brought for consultation and diagnosed to be having HTN and was prescribed on ANTI HYPERTENSIVE DRUGS (on irregular medication) then he had multiple episodes of DRY COUGHsince 8 months
he had FEVER which has been associated with chills and rigor on and off since 8 month 3 episodes
H/O SLURRING OF SPEECH SINCE 1 DAY
H/O TIGHTNESS OVER 4 LIMBS SINCE 1 DAY .
H/O ALTERED SENSORIUM SINCE 2 days
Patient was taken to hospital today morning and was taken to higher center with spo2 68% at RA.
H/o palpitations, sweating when ever he had fever history.
No h/o chest pain
NO LOSS OF WEIGHT AND APETITE.
PAST HISTORY:
Patient is known case of COPD since 1 year
Known case of HTN 1 year ( TELMA 10 MG )
S/P RIGHT FEMUR PFN IN 2012.
8/2/22 - hospital medications prescribed
FAMILY HISTORY:
Not significant
PERSONAL HISTORY:
CHRONIC SMOKING HISTORY SINCE 30 years young age stopped 10 years ago with 1 pack per day
Ocassional alcoholic
GENERAL EXAMINATION:
Patient is conscious, coherent, co operative
Vitals at admission :
GCS : E1V1M1
Temperature: 98F
Pulse rate : 36 BPM
Respiratory rate: 10Cpm
BP : Not recordable
Spo2 : 68% at RA
Cardiovascular system:
S1, S2 heard
No murmurs
Respiratory system: SILENT CHEST
Per abdomen :
Soft , non tender
Bowel sounds present
Central nervous system : LEVEL OF CONCIOUSNESS -COMA
SPEECH - APHASIC.
INVESTIGATIONS:
MDCT SCAN BRAIN - PLAIN
FINDINGS - OLD LACUNAR INFARCT IN LEFT THALAMUS , BILATERAL LENTIFORM NUCLEUS , RIGHT INTERNAL CAPSULE , LEFT CORONA RADIATA.
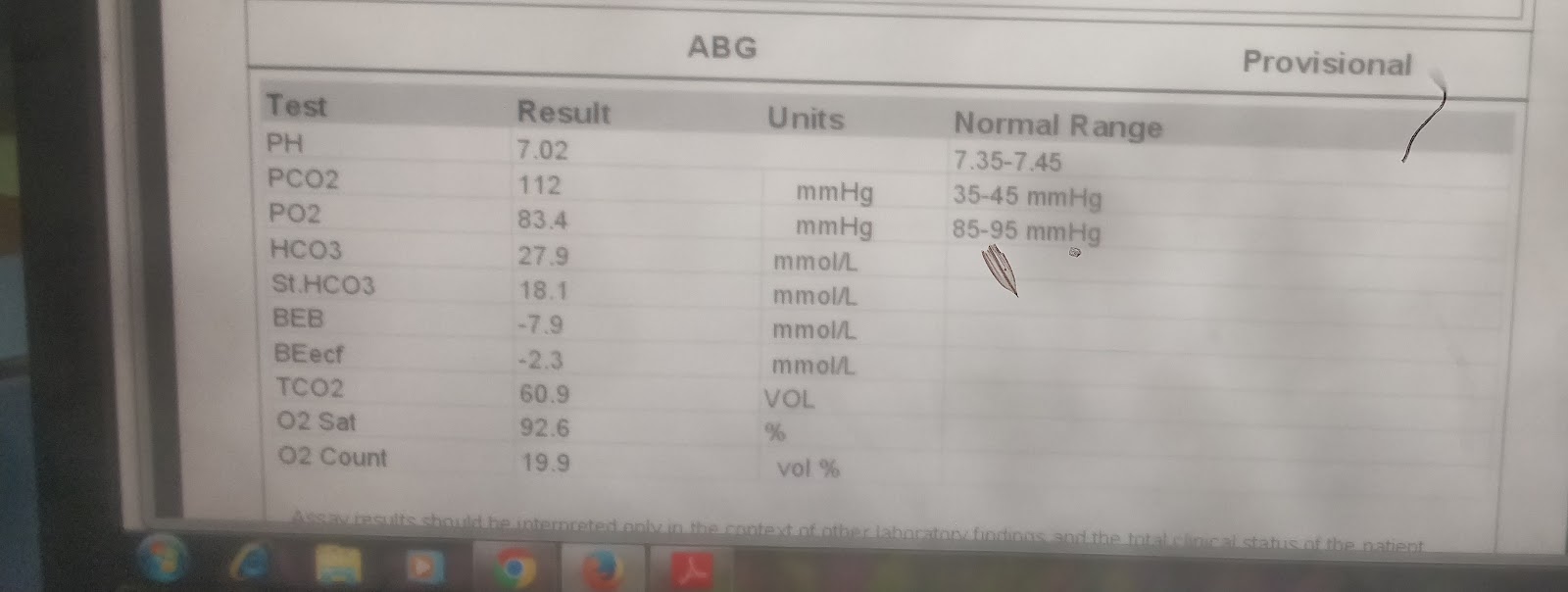
Arterial blood gas : 4/5/22 - 2:16 pm
5/5/22 - 1:57 pm
5/5/22 - 2:18pm
5/5/22 - 10:30 pm
pH -7.224
pCO2 -64.7mm hg
pO2 - 326mm hg
ctHb - 13.5g/dL
sO2 -98.7%
cHCO3 - 22.1mmol/L
cNa+ - 133 mmol/L
cK+ - 3.4 mmol/L
cCa+ - 0.52 mmol/L
cCl- - 92 mmol/ L
6/5/22 - 4:31 am
7/5/22 - 6:42 am
7/5/22 - 11 :56 am
9/5/22 - 5:36 pm
COMPLETE BLOOD PICTURE -
Haemoglobin -12.4gm/dL
Total count - 10,200cells/cumm
Neutrophils -84
lymphocytes-13
Eosinophils-01
Monocytes -02
Basophils -00
Platelet Count - 2.19 lakhs/cu.mm
9/5/22
ESR - 20 mm/ 1st hour
PROTHROMBIN TIME - 20 SEC
INR - 1.4
BLEEDING TIME - 2 MIN
CLOTTING TIME - 4 MIN 30 SEC
APTT - 38 SEC
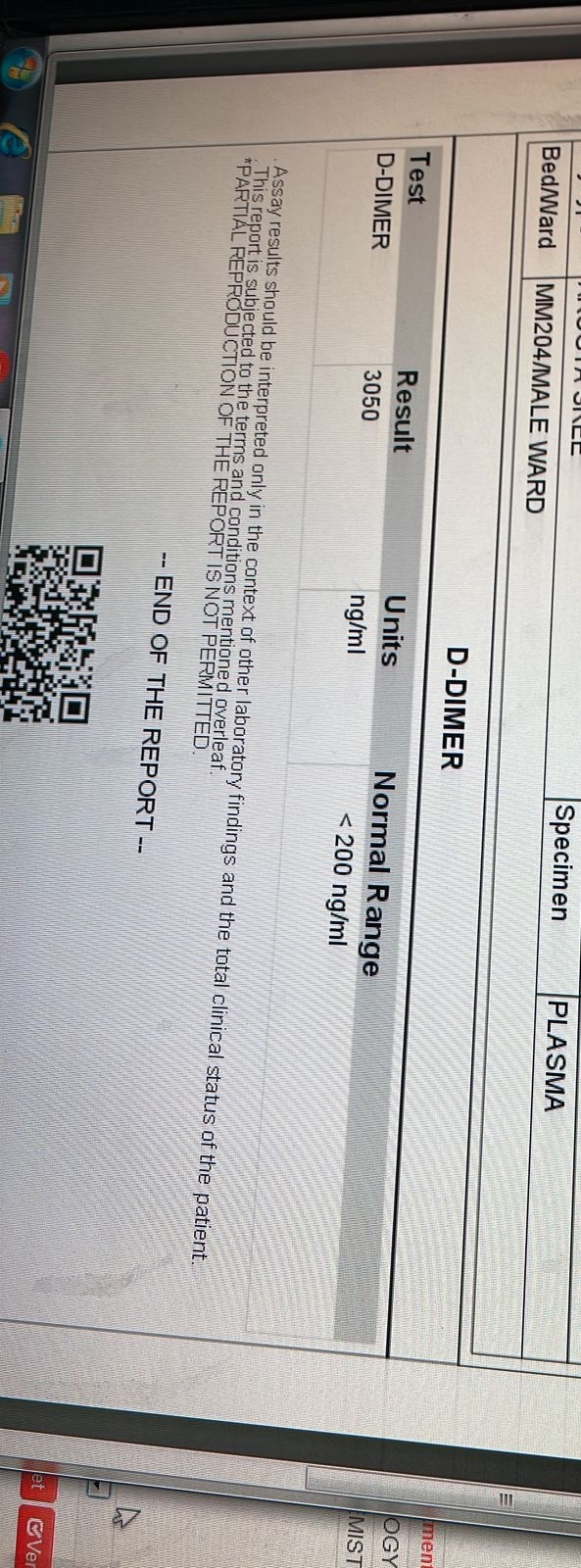
D DIMER - 12,530 ng/ml
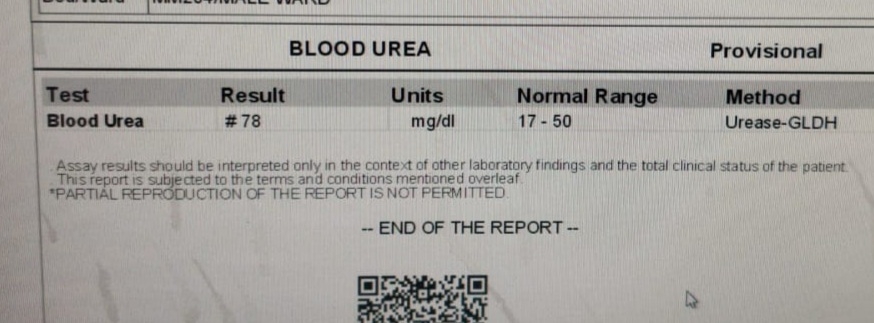
7/5/22 rft5
CHEST X RAY -
CHEST X RAY IMMEDIATELY AFTER INTUBATION -
Urine protien/creat ratio 6/5/22
Urine electrolytes 7/5/22
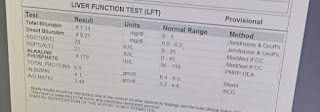
SERUM URIC ACID,SERUM CREATININE , BUN, BLOOD UREA - 6/5/22
TROP I - 115.6 pg/ml
ECG
1:05 pm
D dimer 9/5/22
Blood grouping and RH type :
A POSITIVE
PROVISIONAL DAIGNOSIS - Respiratory acidosis secondary to(resolving) acute exacerbation of COPD with altered sensorium secondary to CO2 narcosis with past h/o HTN ?post cpr inducedvhemopneumothorax with s/p rt sided chest drain insitu.
TREATMENT GIVEN - PATIENT HAS BEEN INTUBATED WITH MIDAZOLAM AND SCOLINE.
CPR WAS STARTED IMMEDIATELY AT 1:10 PM AFTER INTUBATION CONSECUTIVELY WITH 4 CYCLES WITH INJ ADRENALINE 1 MG AND WAS RESUSCITATED 4TH TIME AND HE IS CONNECTED ON MECHANICAL VENTILATION.
TUBE THORACOSTOMY WAS DONE AT 5TH ICS IN MID AXILLARY LINE AND INTERCOSTAL DRAIN OF 24 F WAS PLACED.
1 INJ HYDROCORT 100 MG /IV/TID
2 NEB WITH DUOLIN ABD BUDECORT 2ND HOURLY
3 INJ PIPTAZ 4.5 GM IV/STAT followed by TID
4 INJ PAN 40 MG IV / OD
5 INJ OPTINEURON 1 AMP IN 100 ML NS /IV /OD
6 INJ HEPARIN 5000 IV/QID
7 BP, PR , SPO2 MONITORING
8 ET AND ORAL SUCTIONING EVERY HOURLY.
Soap notes day 1 icu bed no 3
S- no fresh complaints
O-
O/E pt on mechanical ventilator
Bp: 140/80 mm hg
Pr: 77 bpm
Rr: 20 com
Cvs :s1s1 +
Rs: BAE+
P/A: soft , nontender
Grbs: 154mg/dl
I/O = 1100/200
Ventilator settings:
ACMV-VC mode
Rr: 20/min
FIO2: 60
PEEP: 5
VT: 400
A
Respiratory acidosis secondary to(resolving) acute exacerbation of COPD with altered sensorium secondary to CO2 narcosis with past h/o HTN with past h/o COPD with post cpr inducedvhemopneumothorax with s/p rt sided chest drain insitu
P:
Rx:
1.inj hydrocort 100 mg /iv/tid
2.neb with duolin , budecort 2nd hrly
3. Inj piptaz 4.5 mg iv/ TID .
4. Inj pan 40 mg iv/od
5. Inj optineuron 1 aml in 100 ml ns iv /od (over 30 min)
6. Bp,pr ,spo2 monitoring hrly
7. ET oral suctioning every hrly
8.inj heparin 5000iv /od

















































Comments
Post a Comment